Utah-Stanford Ventilator (Vent4US): Developing a rapidly scalable ventilator for COVID-19 patients with ARDS
Posted on: 16 May 2020
Preprint posted on 22 April 2020
Science and engineering meets disease: re-directing talents and ideas towards public health.
Selected by Mariana De NizBackground
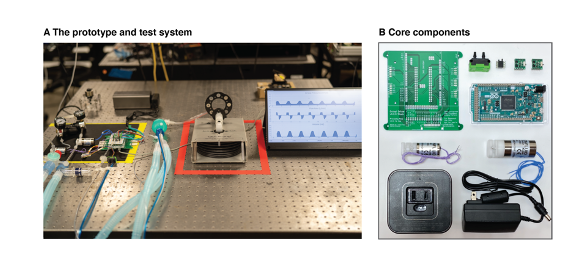
The current global pandemic of the COVID19 respiratory disease caused by the SARS-CoV2 virus has spread rapidly across the world. Many of the patients admitted to intensive care units, present hypoxemic respiratory failure due to severe acute respiratory distress syndrome (ARDS). In many of these cases, the clinical management involves intubation and mechanical ventilation for several days. However, a major concern is that there is a shortage of ventilators worldwide, particularly in developing nations, which is feared to result in the impossibility of providing the required care. Moreover, the production capacity of this life-saving item and its various components, is believed to be insufficient to meet current demand. To address this major public health issue, Li et al developed a minimal ventilator (Figure 1) for use in patients, which has a modular design, and allows use of parts from non-traditional supply chains.
Key developments
Following examination of guidelines published by governments, non-governmental organizations and clinical sources, the authors generated a minimum, modular, rapidly scalable ventilator designed for COVID-19 patients with ARDS. They identified six key requirements of such ventilator to guide their design including a) achieving lung-protective ventilation with low tidal volume; b) measuring and keeping inspiratory plateau pressure at levels within a lung protective strategy; c) set positive end-expiratory pressure to maximize and maintain alveolar recruitment for improved oxygenation; d) provide mechanical support for patient-initiated breaths; e) use respiratory rates of up to 30 breaths/minute; and e) safety measures to lower the risk of barotrauma rebreathing, hypoxia and hypoventilation. The system can be used with compressed medical air or oxygen provided by central hospital supply lines or cylinders.
The authors also generated software that allows setting ventilation parameters, and made the code used for the microcontroller firmware and the graphical user interface, publicly available. They point out that for deployment, various human-machine interfaces are possible, allowing easier implementation. In this preprint the authors go on to discuss next steps including in-depth characterization of the system in terms of space it can operate in, and generating a more complete system with components that can still be integrated. So far, the cost of this ventilator is calculated at around 500 USD, which serves further, the purpose of accessibility by as many people as possible.
What I like about this preprint
I like this preprint because everyone worldwide is making efforts to a huge extent, against the COVID-19 pandemic. Clinicians, nurses, paramedics and other personnel trained in public health or medicine, worldwide are at the frontline of the efforts against this pandemic. Biomedical scientists have brought forward great efforts as well, using their expertise for bridging gaps in aspects such as testing, diagnosis, serology. I like this paper, because work from the Prakash lab has always in the past aimed to increase accessibility to science with designs such as the Foldscope, the BiteOscope, and more recently, the PlanktonScope. I find it exciting that beyond curiosity driven science and promoting its openness and accessibility, the group was able to quickly identify a possibility to help in a global health crisis and again bridge an important accessibility gap, both in terms of the chain of production, and the cost.
Open questions
- Apart from the need of ventilators, you discussed also the burden to the supply chain, and this might include parts of ventilators currently in use. Can some of the parts that you are designing for the ventilator, be used in other models of ventilators – including those currently in use which might need prompt repairs or part replacements?
- What was the biggest challenge you identified, from the timeline between identifying the need for ventilators, and building an initial finalized prototype?
- As part of your discussion, you mention that by making and the designs steps of the prototype open, this is an open door for scientists worldwide contributing with ideas and designs. Has this been the case? Has there been additive collaboration among various labs designing various items, software and pieces of equipment with life-saving potential in this health crisis?
References
- Li H, Li E, Krishnamurthy D, Kolbay P, Chacin B, Hoehne S, Cybulski J, Brewer L, Petelenz T, Orr J, Sakata D, Clardy T, Kuck K, Prakash M, Utah-Stanford Ventilator (Vent4US): Developing a rapidly scalable ventilator for COVID-19 patients with ARDS, bioRxiv, 2020.
doi: https://doi.org/10.1242/prelights.20712
Read preprint










 (No Ratings Yet)
(No Ratings Yet)